What is Osteoarthritis?
Osteoarthritis is a kind of arthritis that is very common and affects millions of people around the world. When the protective cartilage that cushions the ends of the bones breaks down over time, it causes this condition. Although osteoarthritis can affect any joint, it is most typically seen in the hands, knees, hips, and spine. Although the damage to joints cannot be undone, the symptoms of osteoarthritis can typically be treated. Staying active, eating a nutritious diet, and receiving some treatments may help reduce disease development and improve pain and joint function. Take a look at the most common symptoms of Osteoarthritis, also its causes, risk factors, and treatments in detail.
Most Common Symptoms of Osteoarthritis
Osteoarthritis symptoms typically appear gradually and worsen over time. The following are some of the signs and symptoms of osteoarthritis:
-
Pain: The affected joints may pain during or after movement.
-
Stiffness: Joint stiffness may be more obvious when you first wake up or after a period of inactivity.
-
Tenderness: When you apply light pressure to or near your joint, it may become tender.
-
Decreased Flexibility: It's possible that you won't be able to move your joint completely across its range of motion.
-
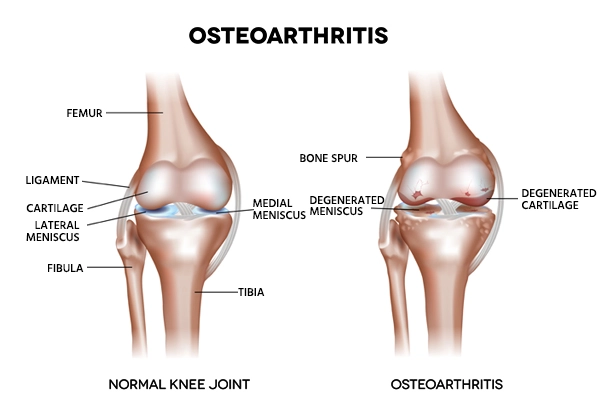
Bone spurs: These extra fragments of bone might grow around the afflicted joint and feel like hard lumps.
-
Swelling: This could be due to inflammation of the soft tissues around the joint.
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second Opinion
Causes of Osteoarthritis
Osteoarthritis develops when the cartilage cushions the ends of bones in joints and deteriorates over time. Cartilage becomes firm, slick tissue that allows for practically frictionless joint movement.
If the cartilage is fully worn down, the bone will rub against the bone. Osteoarthritis is sometimes referred to as a wear-and-tear condition. However, osteoarthritis affects the entire joint, not only the cartilage. It causes bone alterations and the connective tissues that hold the joint together and cause muscle to bone to deteriorate.
Risk Factors of Osteoarthritis
The following are some of the factors that can raise your risk of osteoarthritis:
-
Older age: Osteoarthritis becomes more common as people get older.
-
Gender: Women are more prone than men to get osteoarthritis, while the reason for this is unknown.
-
Stress on the joint on a regular basis: If your profession or an activity you participate in puts repetitive stress on a joint, that joint may develop osteoarthritis over time.
-
Genetic: Osteoarthritis is a condition that some people inherit.
-
Deformities of the bones: Some people are born with faulty cartilage or deformed joints.
-
Some metabolic disorders: Diabetes and an overabundance of iron in the body are two examples (hemochromatosis).
Diagnosis of Osteoarthritis
During the physical exam, your doctor will look for soreness, edema, redness, and flexibility in the afflicted joint. Following are tests for diagnosis
-
X-rays: Cartilage loss is shown by a narrowing of the area between the bones in your joint, which is not visible in X-ray pictures. Bone spurs around a joint can also be seen on an X-ray.
-
Magnetic resonance imaging (MRI): An MRI produces comprehensive images of bone and soft tissues, including cartilage, using radio waves and a strong magnetic field. An MRI isn't always required to diagnose osteoarthritis, although it can provide additional information in some circumstances.
-
Blood tests: Although no blood test exists to diagnose osteoarthritis, certain tests can help rule out other causes of joint pain, such as rheumatoid arthritis.
-
Fluid analysis of the joints: A needle may be used by your doctor to collect fluid from an inflamed joint. The fluid is then examined for inflammation to see if your discomfort is due to gout or infection instead of osteoarthritis.
Treatment for Osteoarthritis
For treating and managing osteoarthritis medicines and therapies are prescribed and when these two methods do not lead to betterment then surgery is suggested.
-
Medications: For treating Osteoarthritis medications are prescribed such as acetaminophen (Tylenol, various brands) for mild to moderate osteoarthritis pain, nonsteroidal anti-inflammatory medicines (NSAIDs) for inflammation, and duloxetine for chronic pain.
-
Physical therapy: It is a type of treatment in which a physical therapist will prescribe some exercises to strengthen the muscles surrounding the joints, promote flexibility, and lessen pain. Regular mild exercise, such as swimming or walking, will promote easy movement.
-
Occupational therapy: It is a term used to describe a type of treatment where an occupational therapist will assist in figuring out how to perform regular tasks without aggravating an already painful joint. If you have osteoarthritis in your hands, for example, a toothbrush with a large handle may make cleaning your teeth simpler.
-
TENS (transcutaneous electrical nerve stimulation): It is a type of electrical nerve stimulation that is used to treat pain, a low-voltage electrical current is used. Some people with knee and hip problems find it helpful in the short term.

Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Therapy
Surgery and Procedures
If medications and conservative therapy are ineffective, then the doctor will prescribe some surgeries like
-
Cortisone injections: This injection is given into the joint that may reduce discomfort for a few weeks. Your doctor numbs the region around the joint before injecting medication through a needle into the joint space.
-
Injections of lubricant: Hyaluronic acid injections may help reduce discomfort by providing cushioning in the knee. Hyaluronic acid is a substance that is naturally found in joint fluid.
-
Realignment of bones: An osteotomy may be beneficial if osteoarthritis has injured one side of your knee more than the other. A surgeon performs a knee osteotomy by making an incision through the bone above or below the knee and then removing or adding a wedge of bone.
-
Joint replacement: It is a procedure that involves replacing a joint. A surgeon will remove the damaged joint surfaces and replace them with plastic and metal pieces during joint replacement surgery. Infections and blood clots are two surgical hazards.