What Is Pericarditis?
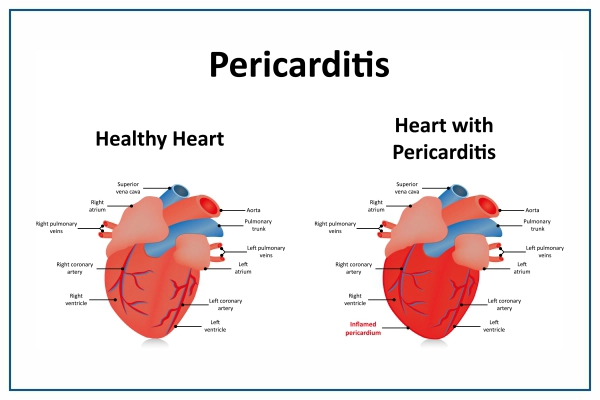
Pericarditis is the inflammation and swelling of the thin, sac-like tissue surrounding the heart (pericardium). It causes very sharp chest pain because the inflamed layers of the pericardium rub against each other.
Pericarditis is usually mild and resolves on its own. Medication and, in rare situations, surgery may be used to treat more severe cases. Early detection and treatment of pericarditis can help in lowering the risk of long-term consequences.
Symptoms of Pericarditis
The most common pericarditis symptom is chest discomfort. It frequently gives a sharp or stabbing sensation. Some patients, however, experience dull, achy, or pressure-like chest pain, which is most commonly felt behind the breastbone or on the left side of the chest, neck, left shoulder or arm. The discomfort may increase due to:
- Pain during swallowing
- Coughing, reclining down or taking a big breath make it worse.
- Wrong sitting or leaning forward habits.
Pericarditis can also cause the following signs and symptoms:
- Cough
- Fatigue
- Swelling of the legs
- Fever of a low-intensity
- Heart pounding or racing (heart palpitations)
- When lying down, you may have shortness of breath.
- Epigastric pain and upper abdominal pain
The symptoms of pericarditis vary depending on the type. It is classified into several types based on the pattern of the symptoms and the duration of symptoms.
- Acute pericarditis appears rapidly and lasts for three weeks or less. Future episodes are possible. It can be difficult to distinguish acute pericarditis from pain caused by a heart attack.
- Recurrent pericarditis develops four to six weeks following an acute pericarditis episode, with no symptoms in the interim.
- Persistent pericarditis usually lasts four to six weeks but no longer than three months. The signs and symptoms do not stop.
- Chronic constrictive pericarditis is characterised by a gradual onset and a duration of more than three months.
When To See The Doctor?
If you acquire new chest discomfort symptoms, seek medical attention right away.
Pericarditis has several symptoms that are similar to those of other heart and lung diseases. If you experience any form of chest pain, it's critical to see a doctor for a comprehensive examination.
Get the best treatment for Pericarditis from the best doctors at Medicover Hospitals.
Cause and Risk Factors of Pericarditis
Various reasons and factors can cause pericarditis:
- After a heart attack or heart surgery, the immune system responds to the damage to the heart (Dressler syndrome, also called postmyocardial infarction syndrome or postcardiac injury syndrome)
- Viral Infections such as COVID-19 or coronavirus infection
- Lupus and rheumatoid arthritis are examples of inflammatory diseases that can lead to pericarditis.
- A heart or chest injury can cause pericarditis
- Kidney failure and cancer are two more chronic health issues that show up with pericarditis as well.
- Malignancy and post-radiation therapy are additional causes of pericarditis.
What Are The Prevention of Pericarditis?
Pericarditis does not have a specific treatment. However, the following precautions to prevent infections may help minimise the risk of heart inflammation.
- Stay away from people who have viral or flu-like sickness. If you have symptoms of a viral infection, try to stay away from others.
- Maintain a healthy level of hygiene. Hand washing on a regular basis can help prevent the spread of sickness.
- Vaccines are highly recommended. Maintain current vaccinations, including those that protect against COVID-19, rubella, and influenza, all of which can cause myocarditis.
Diagnosis of Pericarditis
A doctor would usually examine you and ask questions about your symptoms and medical history to diagnose pericarditis.
To listen to heart sounds, a stethoscope is usually placed on the chest and back. A pericardial rub is a sound produced by pericarditis. When the two layers of the sac enclosing the heart (pericardium) brush against each other, a noise is produced.
Typically, blood tests are performed to look for indicators of a heart attack, inflammation, or infection. Other tests for pericarditis diagnosis include:
- ECG: An electrocardiogram (ECG) is a painless and rapid test that records electrical signals in the heart. Sticky patches (electrodes) connected to wires are placed on the body to monitor these impulses. The data is stored in a computer and displayed as waves on a monitor or paper.
- X-ray of the chest: An X-ray of the chest can reveal changes in the size and shape of the heart. It can aid in the detection of an enlarged heart.
- Echocardiogram: Ultrasound waves create images of the beating heart. Echocardiography can reveal how effectively the heart pumps blood and whether fluid has accumulated in the tissue surrounding the heart.
- Computerized tomography (CT): X-rays are used to create pictures of the heart and chest in cardiac CT scans. The test can detect cardiac thickening, which could indicate constrictive pericarditis.
- Magnetic resonance imaging of the heart (MRI): MRI creates cross-sectional images of the heart using a magnetic field and radio waves. An MRI examination of the thin tissue surrounding the heart can indicate thickening, inflammation, or other alterations.
Treatment
Treatment for pericarditis depends on the origin and degree of symptoms. Mild pericarditis may improve without treatment.
Strenuous activity restrictions should be maintained for 1 to 3 weeks.
- Medications: Anti-inflammatories and anti-swelling medications are frequently administered for treating this condition. Pain relievers like colchicine (colcrys, mitigare) or corticosteroids are recommended.
- Surgical treatments or other procedures: If pericarditis causes fluid to build up around the heart, the fluid may need to be drained through surgery or another method. Pericarditis can be treated with surgery or other techniques such as:
- Pericardiocentesis: A sterile needle or a tiny tube (catheter) is used to extract and drain excess fluid from the pericardial chamber during this treatment.
- Pericardiectomy: The pericardium is removed, if the sac enclosing the heart is chronically stiff owing to constrictive pericarditis, the entire pericardium may need to be removed.
- Refractory causes: Azathioprine IU 1g
Lifestyle changes and self-care
Rest and over-the-counter pain medications, taken as instructed by your healthcare professional, may be all that's required for mild pericarditis.
Avoid excessive physical activity and competitive sports while you recover. Pericarditis symptoms might be triggered by such exercise. Inquire with your doctor about how long you should rest.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Dos and Don’ts
This condition requires proper treatment and a set of do’s and don’ts to be followed to manage it and its related symptoms and infections. During and even after the treatment, one needs to remain aware and alert to manage it better.
Follow the above tips and immediately inform the doctor if there are new pain or symptoms.
Pericarditis Care at Medicover Hospitals
At Medicover Hospitals, we have the most trusted team of cardiology experts who are experienced in providing excellent healthcare services to patients with compassionate care. Our diagnostic department is equipped with modern technology and equipment to conduct the tests required for the diagnosis of Pericarditis. Based on these results, a dedicated treatment plan is designed. We have an excellent team of cardiologists and cardiac surgeons who diagnose and treat this condition with utmost precision, resulting in successful treatment outcomes.