Left Ventricular Assist Devices (LVAD): Indications & Recovery
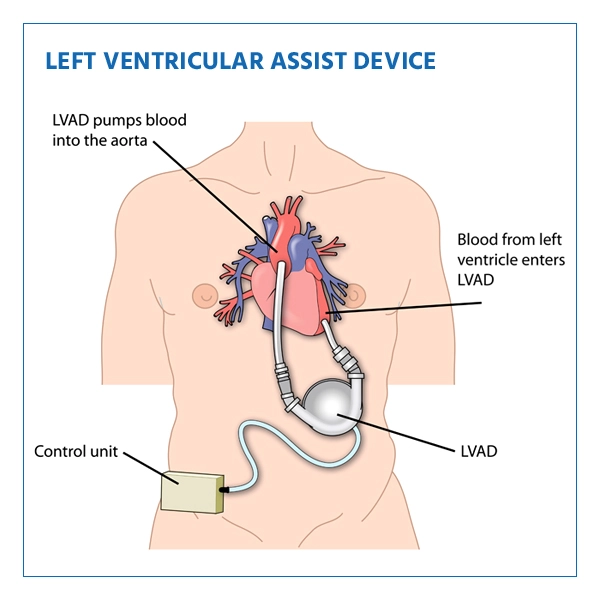
A Left Ventricular Assist Device (LVAD) is a mechanical pump that is surgically implanted into the patient's chest to help a weakened or failing heart pump blood more effectively. It assists the left ventricle in pumping oxygen-rich blood from the heart to the rest of the body.
The procedure involves attaching the LVAD to the heart's left ventricle and aorta, and it can be used as a bridge to heart transplantation or as destination therapy for patients who are not eligible for a heart transplant.
Indications of LVAD-Implantation Procedure
LVAD implantation is indicated for individuals with advanced heart failure whose heart is unable to pump blood effectively. Some common indications include:
- End-stage heart failure
- Severe cardiomyopathy
- Ineligible for heart transplant due to various reasons
- Temporary support while waiting for a suitable heart transplant (bridge to transplant)
- Destination therapy for patients who are not candidates for heart transplantation
- The primary purpose of an LVAD is to provide mechanical circulatory support, improving blood flow, relieving symptoms of heart failure, and enhancing the patient's quality of life.
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second OpinionWho Performs The LVAD Implantation Procedure
The implantation of an LVAD is a highly specialized procedure that requires a team of experts:
- Cardiothoracic Surgeons: These cardiothoracic surgeons perform the implantation surgery.
- Cardiologists: The Cardiologists assess the patient's heart condition and eligibility for LVAD implantation.
- Heart Failure /Transplant Centers: These centers are experienced in managing advanced heart failure and may offer LVAD implantation as a treatment option.
- Referring Physicians: Your primary care doctor or cardiologist can refer you to a specialist if an LVAD is needed.
Preparing for LVAD Implantation Procedure
Before the implantation of an LVAD, several steps are necessary to ensure a successful outcome:
- Consultation and Evaluation: Meet with your cardiologist and surgeon to assess your overall health, medical history, and heart condition.
- Medical Tests: You will undergo tests like blood work, imaging scans (echocardiograms, angiograms), and a physical exam.
- Educational Sessions: Learn about the LVAD device, its function, and what you can expect during and after the procedure.
- Nutrition and Medications: Regularly follow the nutrition guidelines for a balanced diet and review medications.
- Physical Conditioning: It will Depends on your health,The healthcare provider may recommend pre-surgery exercises to build strength.
- Psychosocial Evaluation: Emotional readiness is crucial for adjusting to life with an LVAD, and support services may be offered.
- Advanced Directives: Discuss your healthcare preferences with family or caregivers to ensure that they are respected.
What Happens During LVAD Implantation Surgery?
The LVAD implantation surgery is a complex procedure performed by a team of specialized cardiothoracic surgeons and support staff. Here's an overview of the steps involved:
- Anesthesia: You will be given general anesthesia to ensure you are asleep and pain-free during the surgery.
- Surgical Incision: The surgeon will make an incision in your chest to access your heart. The incision is typically made in the middle of your chest or on the left side.
- Connection to Heart: The surgeon will expose your heart and make connections to the left ventricle, aorta, and possibly the right atrium. Tubes are attached to these areas to facilitate blood flow.
- Implantation of LVAD: The LVAD device is implanted near the heart. One end of the device is connected to the left ventricle, while the other end is connected to the aorta. The device will assist your heart in pumping blood.
- Driveline Placement: A driveline, a thin cable that powers the LVAD, is tunneled through your skin and attached to the device. It exits your body, allowing connection to an external power source.
- Suturing and Closure: The incision is carefully sutured and closed, and sterile dressings are applied.
- Post-Surgery: After surgery, you will be closely monitored in the intensive care unit (ICU). The LVAD team will ensure the device is functioning properly and that your body is adapting to the new setup.
LVAD Complications and Risks
Like any major surgery, LVAD implantation comes with risks and potential complications:
- Infection: There’s a risk of infection at the driveline exit site or within the heart.
- Blood Clots: Blood clots can form and lead to stroke or other complications.
- Bleeding: Patients are at risk of bleeding during or after surgery.
- LVAD Malfunction: The device could fail to pump blood effectively, requiring adjustments or even replacement.
- Thrombosis or Device Obstruction: Blockage or clotting in the device can impede blood flow.
- Heart arrhythmias: The LVAD can cause abnormal heart rhythms that require medical attention.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an AppointmentRecovery After LVAD Implantation Surgery Procedure
Recovery after LVAD implantation surgery is a significant process that involves adjusting to the new device and regaining strength. Here's what to expect during your recovery:
- ICU Stay: After surgery, you will remain in the ICU for monitoring. Vital signs, device function and comfort levels are closely observed.
- Gradual Awakening: As anesthesia wears off, you will gradually regain consciousness and may feel groggy initially.
- Pain Management: Medications are provided to manage pain and discomfort during recovery.
- LVAD Function Monitoring: The LVAD team will ensure the device is working correctly.
- Physical Therapy: Light exercises and movements are introduced to help regain strength and mobility.
- Regular Follow-Up: You'll have frequent follow-up appointments with your LVAD team to monitor your progress and make any necessary adjustments.
Lifestyle Changes After LVAD Implantation Surgery Procedure
After receiving an LVAD, specific lifestyle changes are necessary to ensure your well-being and the longevity of the device. Here are some considerations:
- Medication Adherence: Regular medications to prevent clotting infection, and manage heart function.
- Physical Activity: Engage in recommended activities that strengthen the heart and overall health.
- Heart-Healthy Diet: Consume a balanced diet to support heart health and maintain a healthy weight.
- Device Monitoring: Learn how to monitor the alarm's power supply and respond appropriately to any alerts.
- Emotional Support: Ongoing emotional care and support groups are essential for coping with life post-implantation.
- Regular Follow-Ups: Attend all scheduled follow-up appointments with your LVAD team to ensure the device's proper function and address any concerns.
