What is Mitral Valve Replacement?
The mitral valve, a crucial component of the heart's intricate machinery, plays a vital role in maintaining blood flow between the left atrium and ventricle. When this valve becomes damaged or diseased, it can disrupt the heart's efficiency, leading to various cardiovascular issues. Mitral valve replacement emerges as a transformative solution in such cases.
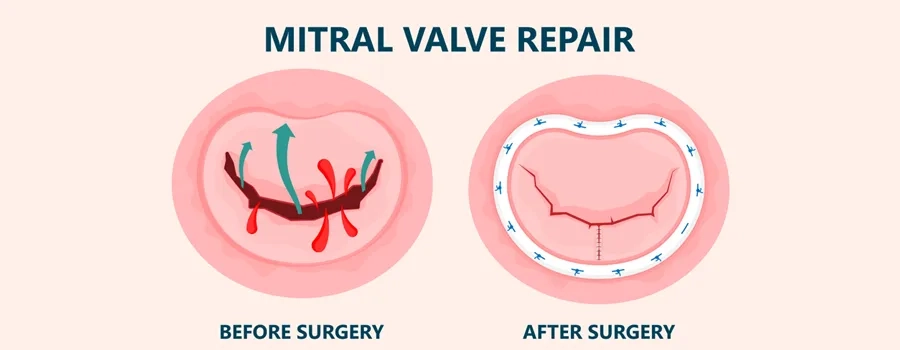
Mitral valve replacement is a surgical procedure that involves replacing a malfunctioning mitral valve with a synthetic valve or a bioprosthetic valve made from animal tissue. This procedure is typically recommended when the valve's function is severely impaired, often due to conditions like mitral valve regurgitation (leakage) or mitral valve stenosis (narrowing).
Mitral valve replacement not only alleviates symptoms like fatigue, shortness of breath, and chest pain but also improves overall heart function and quality of life. Recovery from this procedure varies, but advancements in minimally invasive techniques have contributed to quicker healing times and reduced hospital stays.
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second Opinion
What they do for Mitral Valve Replacement Surgery Procedure
-
Anesthesia: The patient is placed under general anesthesia to ensure they are unconscious and pain-free during the surgery.
-
Incision: A skilled surgeon makes an incision in the patient's chest. The location and size of the incision may vary based on the surgical approach chosen.
-
Cardiopulmonary Bypass (CPB): In most cases, the surgery requires the use of a heart-lung machine, which temporarily takes over the functions of the heart and lungs. The blood is redirected away from the heart, allowing the surgeon to work on the mitral valve in a bloodless environment.
-
Accessing the Heart: The surgeon gains access to the heart through the incision. This can involve separating the sternum (breastbone) and sometimes using rib spreaders to access the heart.
-
Removing the Damaged Valve: The diseased or damaged mitral valve is carefully removed. The surgeon takes care to avoid damaging the surrounding tissues.
-
Preparing the Valve Site: The valve site is carefully inspected and prepared to ensure proper attachment of the prosthetic valve.
-
Prosthetic Valve Placement: The chosen prosthetic valve (mechanical or bioprosthetic) is securely sewn into place at the valve site. The surgeon ensures that the new valve functions properly and allows for optimal blood flow.
-
Closing the Incision: After the prosthetic valve is in place and functioning correctly, the surgeon closes the incision. This may involve sutures, staples, or other closure methods.
-
Weaning from the Heart-Lung Machine: If a heart-lung machine was used, the patient is gradually weaned off the machine, and the heart resumes its normal pumping function.
-
Monitoring and Recovery: The patient is carefully monitored in the postoperative period. They may initially be taken to an intensive care unit (ICU) for close observation before transitioning to a regular hospital room.
-
Recovery and Rehabilitation: As the patient recovers, they may participate in a cardiac rehabilitation program to gradually regain strength, mobility, and cardiovascular fitness.
Indications of Mitral Valve Replacement Surgery Procedure
Indications for mitral valve replacement surgery include:
-
Severe Symptoms: Patients experiencing severe symptoms such as shortness of breath, fatigue, chest pain, or dizziness due to the malfunctioning mitral valve may require surgery.
-
Heart Failure: If the malfunctioning mitral valve is contributing to heart failure, where the heart is unable to pump blood effectively, surgery may be recommended.
-
Valve Stenosis: Severe narrowing of the mitral valve, known as mitral valve stenosis, can impede blood flow from the left atrium to the left ventricle. If medical management is ineffective in relieving symptoms, surgery might be necessary.
-
Valve Regurgitation: Mitral valve regurgitation occurs when the valve doesn't close properly, causing blood to flow back into the left atrium. Severe cases can lead to increased strain on the heart and necessitate surgical intervention.
-
Structural Damage: Structural damage to the mitral valve due to congenital defects, infections, or other conditions may require replacement.
-
Decreased Heart Function: If the heart's pumping function is significantly compromised due to the mitral valve's malfunction, surgery might be needed to improve overall cardiac function.
-
Failed Repair: In some cases, prior attempts to repair the mitral valve might have been unsuccessful, leading to the need for replacement.
-
Chronic Atrial Fibrillation: Long-standing atrial fibrillation (irregular heart rhythm) combined with significant mitral valve dysfunction may necessitate replacement.
-
Deterioration of Biological Valves: If a patient previously had a biological (tissue) mitral valve replacement and it has deteriorated over time, a repeat surgery to replace the valve might be needed.
-
Risk of Complications: Individuals with a high risk of complications related to their mitral valve condition, such as infective endocarditis or severe pulmonary hypertension, might be candidates for replacement surgery.
Who will treat for Mitral Valve Replacement Surgery
-
Cardiothoracic Surgeon: The primary surgeon responsible for performing the mitral valve replacement surgery. They have specialized training in cardiothoracic surgery and extensive experience in performing heart procedures, including valve replacements.
-
Cardiologist: A cardiologist is a medical doctor who specializes in diagnosing and treating heart conditions. They often collaborate with cardiothoracic surgeons to determine the best course of action for patients with mitral valve issues. Cardiologists might also provide preoperative assessments and postoperative care.
-
Anesthesiologist:
Anesthesiologists are responsible for administering anesthesia to ensure the patient's comfort and safety during the surgery. They closely monitor the patient's vital signs and adjust the anesthesia as needed.
-
Perfusionist: Perfusionists operate the heart-lung machine during the surgery. They are responsible for maintaining blood circulation and oxygenation while the heart is temporarily stopped during the procedure.
-
Nurse Practitioners and Physician Assistants: These healthcare professionals play a vital role in patient care before, during, and after the surgery. They assist in patient assessments, education, and postoperative monitoring.
-
Surgical Team: The surgical team includes nurses, scrub technicians, and other specialized personnel who assist the surgeon during the procedure by providing necessary instruments, monitoring the patient's condition, and ensuring a sterile environment.
-
Multidisciplinary Team: In some cases, especially for complex or high-risk surgeries, a multidisciplinary team might be involved. This team could include interventional cardiologists, imaging specialists, radiologists, and other experts who collaborate to make well-informed decisions about the patient's treatment.
-
Rehabilitation Specialists: After the surgery, rehabilitation specialists such as physical therapists and cardiac rehabilitation nurses might help the patient regain strength and cardiovascular fitness during the recovery phase.
How to Prepare for Mitral Valve Replacement Surgery
Preparing for mitral valve replacement surgery involves a combination of medical, logistical, and emotional steps to ensure a smooth and successful procedure. Here's a guide on how to prepare:
-
Consultation with Cardiothoracic Surgeon: Meet with your cardiothoracic surgeon to discuss the procedure, understand its necessity, and address any questions or concerns you may have.
-
Medical Assessment: Undergo a comprehensive medical assessment, which may include blood tests, imaging scans, and electrocardiograms (ECG), to evaluate your overall health and heart condition.
-
Medications: Inform your medical team about all medications, supplements, and herbs you're taking. Some medications might need to be adjusted or temporarily stopped before surgery.
-
Lifestyle Changes: Follow any recommended lifestyle changes, such as quitting smoking, improving your diet, and managing chronic conditions like diabetes or high blood pressure.
-
Preoperative Instructions: Adhere to any preoperative instructions provided by your surgical team, such as fasting before the surgery or using specific antiseptic soaps for hygiene.
-
Mental Preparation: Understand the procedure and its potential benefits and risks. Engage in relaxation techniques, meditation, or counseling to manage anxiety and stress.
-
Logistical Arrangements: Make arrangements for transportation to and from the hospital on the day of surgery, as you may not be able to drive yourself home after the procedure.
-
Hospital Stay Planning: Pack a bag with essential items, including comfortable clothing, toiletries, and any personal items you may want during your hospital stay.
-
Support System: Inform family members or friends about the surgery and recovery period. Having a support system in place can provide emotional and practical assistance.
-
Advance Directives: Consider discussing your wishes for medical care in case of unexpected outcomes. Advance directives, like a living will or healthcare proxy, can ensure your preferences are respected.
-
Diet and Hydration: Follow any dietary instructions given by your surgical team. Staying well-hydrated and having a balanced diet can contribute to better recovery.
-
Home Preparation: Set up a comfortable and organized recovery space at home, including items you may need during your recuperation.
-
Leave of Absence: If you're employed, arrange for the appropriate amount of time off work for your recovery.
-
Final Consultation: Have a final consultation with your surgeon to review the details of the surgery, address any last-minute concerns, and ensure that all preparations are in place.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Recovery after Mitral Valve Replacement Surgery Procedure
Recovery after mitral valve replacement surgery is a gradual process that involves healing, rehabilitation, and adjusting to the changes in your cardiovascular system. Here's what you can expect during the recovery period:
-
Immediate Postoperative Period:
-
Hospital Stay: After the surgery, you'll be closely monitored in the intensive care unit (ICU) for the first few days. Once stable, you'll be transferred to a regular hospital room.
-
Pain Management: Pain and discomfort are normal initially. Your medical team will provide pain medications to manage your discomfort.
-
Monitoring: You'll be continuously monitored for vital signs, heart function, and signs of complications.
-
Chest Tubes and Drains: Temporary chest tubes and drains may be in place to remove excess fluid from the surgical site. These will be removed as your recovery progresses.
-
Days to Weeks Post-Surgery:
-
Mobility and Activity: Gradually, you'll be encouraged to start moving and walking to prevent blood clots, improve circulation, and promote lung function.
-
Breathing Exercises: Deep breathing and coughing exercises help prevent lung infections and clear airways.
-
Diet: You'll start with a liquid diet and gradually transition to solid foods. A balanced diet supports healing.
-
Incision Care: Follow your surgeon's instructions for incision care to prevent infection and promote healing. Keep the incision area clean and dry.
-
Medication Management: Continue taking prescribed medications, including pain relievers and any medications for heart function.
-
Weeks to Months Post-Surgery:
-
Cardiac Rehabilitation: Your healthcare team may recommend a cardiac rehabilitation program to gradually increase your physical activity, improve cardiovascular fitness, and strengthen your heart.
-
Gradual Return to Normal Activities: You'll slowly return to your normal routine, with specific guidance from your medical team. Avoid heavy lifting and strenuous activities initially.
-
Follow-Up Appointments: Regular follow-up appointments with your cardiothoracic surgeon and cardiologist are essential to monitor your recovery and heart function.
-
Medication Adjustments: Over time, your medications may be adjusted based on your progress. It's important to keep track of any changes and report any issues to your medical team.
-
Long-Term Recovery:
-
Scar Care: Proper scar care can help minimize scarring. Follow your surgeon's recommendations for scar treatment.
-
Lifestyle Changes: Continue with any recommended lifestyle changes, such as maintaining a heart-healthy diet, exercising regularly, and managing stress.
-
Medication Management: Depending on the type of valve used (mechanical or bioprosthetic), you might need to take blood-thinning medications or other heart-related medications long-term.
-
Monitor for Changes: Be vigilant about any changes in your health, such as shortness of breath, chest pain, or irregular heartbeats, and promptly report them to your medical team.
Lifestyle changes after Mitral Valve Replacement Surgery Procedure
After undergoing a mitral valve replacement surgery, adopting certain lifestyle changes can contribute to your overall well-being, promote heart health, and ensure the long-term success of the procedure. Here are important lifestyle adjustments to consider:
-
Medication Adherence:
- Take all prescribed medications as directed by your healthcare team. These may include medications for heart function, blood thinners (if required), and other medications to manage specific conditions.
-
Heart-Healthy Diet:
- Limit sodium intake to support blood pressure management.
- Maintain a consistent eating schedule and avoid overeating.
-
Physical Activity:
- Gradually reintroduce physical activity as advised by your medical team.
- Engage in regular aerobic exercises like walking, swimming, or cycling to promote cardiovascular fitness.
-
Tobacco and Alcohol:
- Quit smoking if you're a smoker. Smoking can negatively affect your heart health and interfere with healing.
- Limit alcohol consumption as advised by your healthcare team.
-
Follow-Up Appointments:
- Attend all scheduled follow-up appointments with your cardiothoracic surgeon and cardiologist. These visits help monitor your heart's health and recovery progress.
-
Cardiac Rehabilitation:
- Participate in a cardiac rehabilitation program as recommended by your healthcare team. This program can help you regain strength and cardiovascular fitness under professional guidance.
-
Awareness of Symptoms:
- Be vigilant about any new or worsening symptoms, such as shortness of breath, chest pain, fatigue, or irregular heartbeats. Promptly report any concerns to your medical team.
-
Emotional Well-being:
- Seek emotional support if needed. Connecting with family, friends, or support groups can help you manage the emotional aspects of recovery.
-
Healthy Sleep Habits:
- Aim for 7-9 hours of quality sleep per night. Good sleep supports healing and overall well-being.
-
Medical Alert Bracelet:
- Consider wearing a medical alert bracelet indicating that you have undergone heart surgery. This can be crucial in case of emergencies.