Bleeding is the most serious complication of oral anticoagulation in the prevention and treatment of thromoboembolic complications. Even after NOACs (Novel oral anticoagulants) discovery, Acitrom or Acenocoumarol is the most common oral anticoagulant used in practice. Here we present a case report of Acitrom causing bleeding into intestinal submucosa causing acute pseudo-obstruction.
Case Report:
A 70-yr old female presented with complaints of abdominal bloating, nausea, early satiety, haematuria, increased belching, severe generalized weakness since 3 days, constipation, b/l pedaloedema,abdominal pain and recurrent vomiting since 2days.
She is a known case of Diabetic, Hypertensive, CRHD, status post PBMV and Atrial Fibrillation and was on Acitrom since 5 yrs. At the time of admission, she is Conscious and Coherent. BP: 170/70 mm Hg PR: 96/min, irregularly irregular rhythm, RR: 22/min RBS: 339 mg/dl. TEMP: 98.6°f, SpO2 : 98% at room air. CVS: S1, S2+ Mid diastolic murmur+. RS: BAE+, Clear airways. P/A: Diffuse vague tenderness+. CNS: NAD.
Lab evaluation shows – Hemogram is s/o microcytic hypochromic anaemia, relative neutrophilia. HbA1c is 8%. Renal function tests and Electrolytes were with in normal limits. CUE shows sugar 2+, protein 1+, plenty of RBC ‘s. INR is >100 [N -0.8 - 1.2].
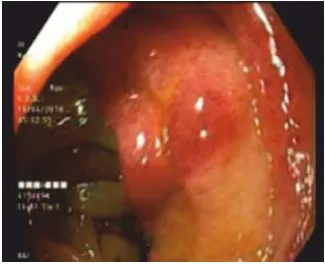
CECT Abdomen done and is s/o Ill-dened non- enhancing hypodensity measuring 8.1 x 2.6 x 3.9 Cm (coronal x sagittal) was seen in endometrial cavity extending into the anterior and posterior wall myometrium, predominantly in the distal body and cervical region without extension into parametrium and vaginal suggestive of Carcinoma. 2D Echo study was s/o moderate mitral stenosis, EF – 52%, Atrial fibrillation. Cardiologist, Surgeon, Gastroenterologist and Gynaecologist consulted. Upper GI Endoscopy was done and suggested ulceration at GE junction, sub mucosal haemorrhages with oedematous mucosa at D1, Cap and D2 region with duodenal obstruction - Acitrom induced (Fig.1). She was kept on Nil by mouth.
Acitrom was withheld in view of high PT/INR. Vitamin K 10mg IV once in a day for 3 days was given. She was treated with empirical Antibiotics, Insulin, Cordarone, Metoprolol,Paracetamol, Proton pump inhibitors, IV fluids and Supportive measures.
She responded well to the above treatment and passed stools 2 days later. INR improved to 3.5 on day 3. Haematuria subsided. She was discharged in stable condition with advice to attend the surgical oncologist. Here, our patient was presented with clinical features suggestive of but radiological features not consistent with intestinal obstruction – making it atypical presentation.
Discussion
Pseudo-obstruction can be Primary or idiopathic and Secondary1. It present in acute or chronic form. Clinical features are abdominal pain, distension, nausea, vomiting, constipation, or diarrhoea and obstipation. It often affects colon more than small intestine and duodenum. It arises from disordered gut motility and is more common in dysmotility states, such as diabetes, amyloidosis, and scleroderma.
Acute colonic pseudo-obstruction, also known as Ogilvie syndrome, most commonly affects the large intestine from the cecum to the splenic flexure. The exact pathophysiology is unknown, but it has been linked to dysregulation of the autonomic nervous system.
It is more common in men and patients over the ages of 60. It is commonly found in hospitalized patients after surgery or after a severe illness. Medications, metabolic imbalances, non-operative trauma, surgery, and cardiac disease have all been associated with intestinal pseudo-obstruction
Chronic intestinal pseudo-obstruction is a more rare form of pseudo-obstruction. Autoimmune disorders like scleroderma, lupus etc, Porphyria, Disorders that affect nerves like Diabetes.
Parkinson’s disease, Medications like Opiates, TCAs, Atropine etc, Paraneoplastic syndromes, Radiation treatment and some viral infections like EBV are known to cause Chronic intestinal pseudo-obstruction.
Pseudo-obstruction is diagnosed based on symptoms, clinical findings, and tests to rule out the presence of a mechanical obstruction. Drug-related pseudo-obstruction remains underreported, but is of importance in modern society where drugs are endemically abused. Thorough evaluation is needed to rule out mechanical obstruction and initial management includes bowel rest, nasogastric decompression, intravenous fluid resuscitation, and treatment of the underlying cause.
Acenocoumarol and the coumarin anticoagulants are structurally similar to vitamin K and competitively inhibit the enzyme vitamin K-epoxide reductase. Hence, they are called vitamin K antagonists.
Oral anticoagulation has become safer in recent years, especially if monitored regularly. Tolerability of Acenocoumarol was similar in younger and elderly population (aged >70 years), with Acenocoumarol being well-tolerated in both the populations. Caution is required especially in elderly patients to prevent bleeding complications and anticoagulation intensity should be closely monitored to reduce periods of overdosing.3 The INR should be reduced to a safe level ( <5) if excessive increase in prothrombin time and/or INR occur without bleeding or prospective surgery. If serious bleeding is present, the INR should be reduced to 1 as soon as possible. If elective surgery or urgent surgery is required, the INR can be reduced to 1 to 1.5 at the time of surgery. INR can be reduced temporarily by withdrawing anticoagulant therapy and, if necessary, administering oral or parenteral vitamin K. When immediate restoration of clotting factors is necessary for serious overdose or life-threatening bleeding, transfusion of fresh frozen plasma or prothrombin (factor IX) complex concentrate along with vitamin K may be necessary.
References
State of Art Technology Mri, Ct. pet-ct And All Oter Diagnostic Services
Contributors
Senior Consultant Physician And Diabetologist
News Letter
Medicover Hospitals Impact Newsletter November 2022