Guillain Barre syndrome masquerading as angina pectoris
Jan 11 2023 | Medicover Hospitals | HyderabadA 45-year-old woman presented to the emergency department complaining of stabbing chest pain radiating to both shoulders, upper back and upper abdomen for the past 3 days. She reported stabbing pain in the chest and upper abdomen associated with postprandial fullness and discomfort. There was no dyspnea but she had nausea, vomiting and diaphoresis. She denied medical history such as diabetes mellitus, hypertension and special personal history. She was initially admitted and evaluated under the care of a cardiologist in another institute and transferred to our hospital later.
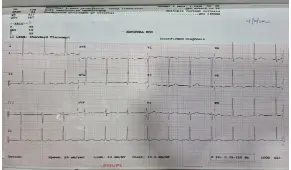
On arrival, examination revealed blood pressure was 140/90 mmHg, heart rate 110 bpm, respiratory rate 26/min and pulse oximetry of 100% on ambient air. She was profusely sweating despite her body temperature being normal. Serial electrocardiograms (ECGs), cardiac injury biomarkers, creatine phosphokinase, electrolytes, and echocardiography were unremarkable. Coronary angiography was contemplated. Neurology consult was sought before coronary angiography as her speech was found to be slurred.
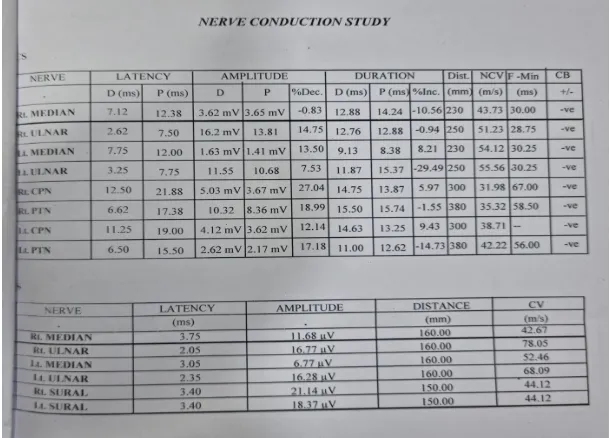
Her neurological exam revealed bilateral facial weakness involving upper as well as lower half of her face. Neck flexion was mildly weak. Upper extremity motor strength and reflexes were normal. Lower extremity strength was decreased, with absent knee and ankle tendon reflexes. Proximal muscles were weaker than the distal ones. Sensations were intact. She was clinically suspected to be a case of Guillain Barre syndrome (GBS). Nerve conduction studies (NCS) showed prolongation of distal motor latencies in both median nerves and both common peroneal nerves, reduction of sensory nerve action potentials (SNAPs) in both median nerves, with normal SNAPs in sural nerves.
The diagnosis of GBS was established supported by the evidence of demyelinating peripheral nerve injury from electrophysiologic testing.
The initial Medical Research Council sum score (MRCss) was 48/60. Thereby, she received a standard dose of intravenous immunoglobulin (IVIG) for five consecutive days. All supportive measures including nutrition and physiotherapy were provided. Her chest pain subsided remarkably after two days of treatment. She started gradually regaining strength in her lower limbs as well. Two weeks following IVIG, she was able to walk independently and her MRCss had improved to 58/60.